It will be highly interesting in future investigations to determine the effects of the seminal plasma-specific posttranslational modifications on PCI functions, such as the inhibition of various proteases and cell-surface receptor interactions. However, protease inhibition experiments will require the isolation of active seminal plasma-derived PCI, which has proven to be very difficult to achieve, due to the high concentrations of serine proteases in seminal plasma. Alternatively, it may be possible to produce recombinant PCI expressing the seminal plasma PCI N-glycans, although this is a difficult task because it requires the precise expression of the correct glycosyltransferases. A recent study indicates that PCI could also play another functional role in the human male and female BU 4061T reproductive systems. The immune lectin designated DC-SIGN is associated with both mature and immature dendritic cells. Many human pathogens bind to DC-SIGN, enabling their VE-822 detection, uptake and the development of specific adaptive immune responses by DCs. However, DC-SIGN also binds to several endogenous glycoproteins, and such interactions are currently thought to promote immune homeostasis. Many proteins are specifically produced in the male urogenital tract after the onset of puberty, but they have not been subjected to thymic education. Such autoantigens could trigger immune responses in both the human male and female reproductive systems. However, PCI and three other glycoproteins have recently been defined as endogenous glycoprotein ligands for DC-SIGN in seminal plasma. Extensive fucosylation was important for these interactions. Therefore seminal plasma PCI could also have an immunomodulatory effect in both the male and female reproductive tracts, in which fucosylation plays a critical role. The results presented here provide further support that posttranslational modifications affect the functional specificity of PCI, which is medically relevant because PCI can act for instance as an anti-inflammatory and antitumor agent. It is also essential for all stages of reproduction. Therefore it may be used for therapeutic purposes. It was previously shown that the overall removal of Nlinked glycans and the NH2-terminal peptide of PCI affect the inhibition rates in the presence but not in the absence of the cofactors heparin and thrombomodulin. For factor Xa, the NH2-terminal peptide of PCI was found to affect the inhibition rates both in the absence and the presence of heparin. PSA, in contrast, is unique in that only  the combination of the N-glycans and the NH2-terminus of PCI affect the rate of its inhibition. Estrogens are important steroidal hormones which exert different physiological functions. The main beneficial effects include their role in programming the breast and uterus for sexual reproduction, controlling cholesterol production in ways that limit the build-up of plaque in the coronary arteries, and preserving bone strength by helping to maintain the proper balance between bone build-up and breakdown. Among female sex hormones, 17b-estradiol is the most potent estrogen carrying out its action either via transactivation of estrogen receptors or by stimulating nongenomic effects via the MAPK signaling pathway. In addition to its important beneficial effects, however, E2 can also cause serious problems arising from its ability to promote the cell proliferation in breast and uterus. Although this is one of the normal functions of estrogen in the body, it can also increase the risk of estrogen dependent diseases, like breast cancer, endometriosis and endometrial hyperplasia. Suppression of estrogenic effects is consequently a major therapeutic approach.
the combination of the N-glycans and the NH2-terminus of PCI affect the rate of its inhibition. Estrogens are important steroidal hormones which exert different physiological functions. The main beneficial effects include their role in programming the breast and uterus for sexual reproduction, controlling cholesterol production in ways that limit the build-up of plaque in the coronary arteries, and preserving bone strength by helping to maintain the proper balance between bone build-up and breakdown. Among female sex hormones, 17b-estradiol is the most potent estrogen carrying out its action either via transactivation of estrogen receptors or by stimulating nongenomic effects via the MAPK signaling pathway. In addition to its important beneficial effects, however, E2 can also cause serious problems arising from its ability to promote the cell proliferation in breast and uterus. Although this is one of the normal functions of estrogen in the body, it can also increase the risk of estrogen dependent diseases, like breast cancer, endometriosis and endometrial hyperplasia. Suppression of estrogenic effects is consequently a major therapeutic approach.
Monthly Archives: August 2019
Injection of SU5416 is found to abrogate EAE in comparison to standard EAE induction with MOG peptide
At the very least, it confirms that a potential endogenous ligand that binds both isoforms equally might exist. Ever since it was reported that some ligands of the AHR favor Treg generation and others favor Th17 differentiation, we  have been categorizing novel ligands for their properties in T-cell differentiation. The above data support that SU5416 enhances Treg generation in vitro, and that IDO is generated in pDCs in response to SU5416 in vitro in an AHR-dependent manner. We continue to characterize these effects for multiple ligands, and are considering theories explaining these differences including the potency and duration of binding of the ligands to the receptor, a possible change in conformation of the receptor when different ligands bind, and a possible effect on APC-T cell interactions. That being said, there is some data to suggest that these dichotomous findings are not as clear cut as originally thought. Most of the in vitro studies examining effects on T-cell PF-04217903 differentiation are done either in Treg or Th17 conditions, which are artificial by design. In addition it has been shown that FICZ, the ligand best associated with Th17 differentiation, can enhance Treg differentiation in the presence of TGF-b, and TCDD can enhance Th17 differentiation. This is similar to the data we show in supplementary figure 4, where SU5416 increases IL-17 in the supernatant of T cells cultured in Th17 conditions at low doses. It is likely that these effects are highly dependent on the ligand, the inflammatory milieu that is present in the assay or disease process, and the particular in vivo model system being studied. The prototypical regulatory ligand is TCDD, although others have been identified. FICZ remains the most well characterized effector ligand. By further delineating the properties of these ligands and the inflammatory milieu that allow them to have disparate effects on T-cell differentiation, it may ultimately be possible to utilize these properties to treat various diseases. This will require more characterization in vitro and in vivo. We do not believe the ligand activity is attributed to an indirect effect driven by VEGF, due to the impressive and rapid competitive binding in the radioligand assay, and additionally because we did test other known inhibitors of VEGFR-2, and did not find consistent DRE-luciferase activity in the range of their activity with VEGFR-2. In addition to and independent of its effect on the AHR, SU5416 is certainly an inhibitor of VEGFR-2, as was well proven in previous studies. The implications of our findings are important both for potential utility of this drug in humans, but also for mechanistic interpretations of previous experiments in vitro and in vivo. Regarding previous in vitro and in vivo studies, there is strong data supporting a role for VEGF in immune cell migration and chemotaxis, generation of inflammatory cytokines, and angiogenesis. With that said, there are numerous studies that utilize SU5416 in experimental models and interpret the results based on its VEGF effect. For example, one recent paper analyzed the role of VEGF in airway inflammation in vitro and in a murine model. The authors found that SU5416 blocked LPS-induced airway inflammation, and specifically the differentiation of T cells to Th17 cells, along with a reduction of IL-6. These data would be fully consistent with regulatory effects of the drug Temozolomide through the AHR. While VEGF may also have a role in this differentiation, these data need to be interpreted carefully. In another study, which is presumed to be due to disruption of the effects of VEGF in this model.
have been categorizing novel ligands for their properties in T-cell differentiation. The above data support that SU5416 enhances Treg generation in vitro, and that IDO is generated in pDCs in response to SU5416 in vitro in an AHR-dependent manner. We continue to characterize these effects for multiple ligands, and are considering theories explaining these differences including the potency and duration of binding of the ligands to the receptor, a possible change in conformation of the receptor when different ligands bind, and a possible effect on APC-T cell interactions. That being said, there is some data to suggest that these dichotomous findings are not as clear cut as originally thought. Most of the in vitro studies examining effects on T-cell PF-04217903 differentiation are done either in Treg or Th17 conditions, which are artificial by design. In addition it has been shown that FICZ, the ligand best associated with Th17 differentiation, can enhance Treg differentiation in the presence of TGF-b, and TCDD can enhance Th17 differentiation. This is similar to the data we show in supplementary figure 4, where SU5416 increases IL-17 in the supernatant of T cells cultured in Th17 conditions at low doses. It is likely that these effects are highly dependent on the ligand, the inflammatory milieu that is present in the assay or disease process, and the particular in vivo model system being studied. The prototypical regulatory ligand is TCDD, although others have been identified. FICZ remains the most well characterized effector ligand. By further delineating the properties of these ligands and the inflammatory milieu that allow them to have disparate effects on T-cell differentiation, it may ultimately be possible to utilize these properties to treat various diseases. This will require more characterization in vitro and in vivo. We do not believe the ligand activity is attributed to an indirect effect driven by VEGF, due to the impressive and rapid competitive binding in the radioligand assay, and additionally because we did test other known inhibitors of VEGFR-2, and did not find consistent DRE-luciferase activity in the range of their activity with VEGFR-2. In addition to and independent of its effect on the AHR, SU5416 is certainly an inhibitor of VEGFR-2, as was well proven in previous studies. The implications of our findings are important both for potential utility of this drug in humans, but also for mechanistic interpretations of previous experiments in vitro and in vivo. Regarding previous in vitro and in vivo studies, there is strong data supporting a role for VEGF in immune cell migration and chemotaxis, generation of inflammatory cytokines, and angiogenesis. With that said, there are numerous studies that utilize SU5416 in experimental models and interpret the results based on its VEGF effect. For example, one recent paper analyzed the role of VEGF in airway inflammation in vitro and in a murine model. The authors found that SU5416 blocked LPS-induced airway inflammation, and specifically the differentiation of T cells to Th17 cells, along with a reduction of IL-6. These data would be fully consistent with regulatory effects of the drug Temozolomide through the AHR. While VEGF may also have a role in this differentiation, these data need to be interpreted carefully. In another study, which is presumed to be due to disruption of the effects of VEGF in this model.
This has reached maturity to the point that we can entertain various viable therapeutic options
Statins have an unparalleled safety and efficacy profile, but often lead to suboptimal levels of LDLc in patients with ADH, show variable patient-dependent responses, and/or result in unwanted side effects, emphasizing the need for other molecules to further lower LDLc. In hepatocytes, statins up-regulate PCSK9 mRNA to a greater extent than LDLR. This revealed the paradox that statins on the one hand enhance LDLR level and activity thereby lowering LDLc, but on the other hand increase the expression of PCSK9 that has the ability to destroy the LDLR and oppose its LDLlowering effect. Therefore, it is believed that neutralization of PCSK9 would enhance the efficacy of statins. Indeed, a significant association of the LOF mutation PCSK9-R46L with statin response was observed in a genome-wide analysis. This supports the hypothesis that the up-regulation of PCSK9 induced by statins attenuates the decrease in LDLc. Lowering PCSK9 levels and/or function has been achieved by antisense mRNA, locked nucleic acids and inhibition of PCSK9;LDLR interaction and degradation using PCSK9 monoclonal antibodies. The latter approach is expensive, restricting it to high risk patients in whom a maximal tolerable dose of statin does not achieve LDLc target levels. Thus, there is a need for cheaper, more accessible  inhibitory small molecules, which are not yet available. Annexin A2 is strongly expressed in lungs, aorta, heart, adrenals and small intestine. Intracellular AnxA2 is part of a heterotetramer complex comprising two AnxA2 monomers and two copies of its natural binding partner, p11. AnxA2 is composed of an N-terminal 23 aa segment that binds p11, followed by four repeat structures. Although lacking a signal peptide, AnxA2 is translocated to the cell surface through a p11-dependent mechanism and is found at the cell surface of epithelial and endothelial cells. As a co-receptor for plasminogen and tissue plasminogen activator, which are required for plasmin generation, the AnxA2 complex promotes vascular fibrinolysis. It was suggested that injection of AnxA2 in human may improve thrombotic disease outcome. AnxA2 knockout mice are viable, but deficient in endothelial plasminogen processing into plasmin and neoangiogenesis. We previously identified AnxA2 as a natural inhibitor of PCSK9’s function on the LDLR, through binding of the first R1 repeat domain of AnxA2 to the CHRD. Inhibition likely occurs via an allosteric PCSK9 conformational change induced by AnxA2, similar to what was reported for mAbs that bind the CHRD. In this report, we investigated in more details the molecular interaction of the R1 domain of AnxA2 and PCSK9 and showed that a synthetic peptide spanning the R1 domain is a potent inhibitor. We further hypothesized that PCSK9 is much more active in enhancing LDLR degradation in AnxA22/2 mice. Indeed, our data showed that AnxA22/2 mice exhibit a higher level of MLN4924 circulating PCSK9 and lower LDLR protein levels in various tissues previously reported to be refractory to PCSK9’s extracellular function on LDLR, such as the adrenals. Furthermore, overexpression of AnxA2 using a recombinant adenovirus resulted in higher LDLR levels in liver. Finally, by sequencing exons of human AnxA2 we identified individuals with a V98L polymorphic variation in the R1 domain, and showed that this variant could be associated with lower levels of circulating PCSK9. The discovery of PCSK9 and its genetic relation to hypercholesterolemia led to a very exciting and active period of identification of the mechanisms of action of PCSK9, and to the BU 4061T development of powerful animal genetic models.
inhibitory small molecules, which are not yet available. Annexin A2 is strongly expressed in lungs, aorta, heart, adrenals and small intestine. Intracellular AnxA2 is part of a heterotetramer complex comprising two AnxA2 monomers and two copies of its natural binding partner, p11. AnxA2 is composed of an N-terminal 23 aa segment that binds p11, followed by four repeat structures. Although lacking a signal peptide, AnxA2 is translocated to the cell surface through a p11-dependent mechanism and is found at the cell surface of epithelial and endothelial cells. As a co-receptor for plasminogen and tissue plasminogen activator, which are required for plasmin generation, the AnxA2 complex promotes vascular fibrinolysis. It was suggested that injection of AnxA2 in human may improve thrombotic disease outcome. AnxA2 knockout mice are viable, but deficient in endothelial plasminogen processing into plasmin and neoangiogenesis. We previously identified AnxA2 as a natural inhibitor of PCSK9’s function on the LDLR, through binding of the first R1 repeat domain of AnxA2 to the CHRD. Inhibition likely occurs via an allosteric PCSK9 conformational change induced by AnxA2, similar to what was reported for mAbs that bind the CHRD. In this report, we investigated in more details the molecular interaction of the R1 domain of AnxA2 and PCSK9 and showed that a synthetic peptide spanning the R1 domain is a potent inhibitor. We further hypothesized that PCSK9 is much more active in enhancing LDLR degradation in AnxA22/2 mice. Indeed, our data showed that AnxA22/2 mice exhibit a higher level of MLN4924 circulating PCSK9 and lower LDLR protein levels in various tissues previously reported to be refractory to PCSK9’s extracellular function on LDLR, such as the adrenals. Furthermore, overexpression of AnxA2 using a recombinant adenovirus resulted in higher LDLR levels in liver. Finally, by sequencing exons of human AnxA2 we identified individuals with a V98L polymorphic variation in the R1 domain, and showed that this variant could be associated with lower levels of circulating PCSK9. The discovery of PCSK9 and its genetic relation to hypercholesterolemia led to a very exciting and active period of identification of the mechanisms of action of PCSK9, and to the BU 4061T development of powerful animal genetic models.
Demonstrated for the first time that short-term treatment with all DPP-4 inhibitors decreases the plasma concentrat
Chronic kidney disease and moreover, end-stage renal disease, have been shown to increase cardiovascular disease and risk of death. This has been substantiated in a systematic review on mortality risk, which concluded that increased risk for all-cause mortality in CKD high content screening supply patients was largely driven by cardiovascular deaths. Glucagon-like peptide-1 is an incretin hormone secreted by the small intestine in response to nutrient ingestion. Although the major physiological function of GLP-1 appears to relate to glycaemic control, evidence suggests that GLP-1 plays an important role in the cardiovascular system. GLP-1 receptors are expressed in the heart and vasculature of rodents as well as humans. Research has shown that GLP-1R agonists BIBW2992 affect a wide range of cardiovascular parameters, including heart rate, blood pressure, vascular tone and myocardial contractility. Importantly, these agents may also have beneficial effects in the setting of cardiovascular disease. For example, GLP-1 has been found to exert cardioprotective actions in experimental models of dilated cardiomyopathy, hypertensive heart disease and myocardial infarction. Preliminary clinical studies also suggest that GLP-1 infusion may improve cardiac contractile function in chronic heart failure patients with and without diabetes, and in MI patients after successful angioplasty. However, the cardiovascular effects of a pharmacological increase in GLP-1 in patients with CKD have not been determined. Dipeptidyl peptidase-4 inhibitors are considered incretin enhancers, because they inhibit the enzymatic degradation of incretins, in particular, GLP-1 and therefore are established therapies for type 2 diabetes. At the same time, DPP-4 inhibition does not cause hypoglycemia, as was previously shown by Bergman et al in a study in healthy male volunteers. Because the action of GLP-1 on insulin secretion is strictly glucose dependent, the risk of hypoglycaemia associated with DPP-4 inhibitors is low.The main elimination route of the first generation of approved DPP-4 inhibitors is via the kidney. Dose adjustment in patients with diabetes and chronic renal failure is thus necessary. Linagliptin a recently launched DPP-4 inhibitor is different in this respect with primary elimination via the bile and only 1-5% eliminated via the urine. We studied the 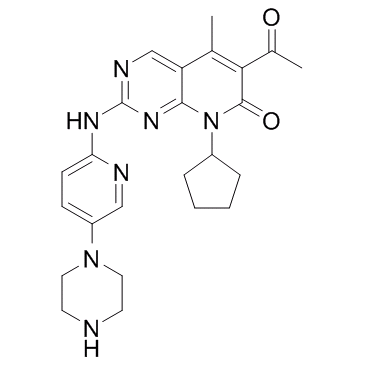 pharmacokinetics and pharmacodynamics of different DPP-4 inhibitors, in the settings of CRF, in order to determine the properties of DPP-4 inhibitors to be used in patients with impaired renal function, and investigated the effects of linagliptin on biomarkers of cardiac and renal fibrosis. The results showed that DPP-4 inhibition increases plasma GLP-1 levels, particularly in uremia, suggesting that linagliptin may offer a unique approach for treating uremic cardiomyopathy in CKD patients. The overall goal of the present study was to compare the pharmacokinetic properties of available DPP-4 inhibitors in a rat model of uremic heart disease and select the optimal compound based on these data for the first pharmacodynamics analyses of potential efficacy in this rat model. We have shown that renal impairment does not affect the pharmacokinetics of linagliptin, whereas it increases the exposure of sitagliptin and alogliptin. In the present study, only linagliptin was found not to further aggravate pathological changes of glomerular and tubular markers in rats with CRF, suggesting that it is a safe approach to be used in patients with CRF. Consequently, linagliptin was also the compound of choice to investigate further effects on uremic cardiomyopathy. This is of potential clinical impact, since patients with advanced stages of renal impairment are characterized by a high overall cardiac morbidity and mortality.
pharmacokinetics and pharmacodynamics of different DPP-4 inhibitors, in the settings of CRF, in order to determine the properties of DPP-4 inhibitors to be used in patients with impaired renal function, and investigated the effects of linagliptin on biomarkers of cardiac and renal fibrosis. The results showed that DPP-4 inhibition increases plasma GLP-1 levels, particularly in uremia, suggesting that linagliptin may offer a unique approach for treating uremic cardiomyopathy in CKD patients. The overall goal of the present study was to compare the pharmacokinetic properties of available DPP-4 inhibitors in a rat model of uremic heart disease and select the optimal compound based on these data for the first pharmacodynamics analyses of potential efficacy in this rat model. We have shown that renal impairment does not affect the pharmacokinetics of linagliptin, whereas it increases the exposure of sitagliptin and alogliptin. In the present study, only linagliptin was found not to further aggravate pathological changes of glomerular and tubular markers in rats with CRF, suggesting that it is a safe approach to be used in patients with CRF. Consequently, linagliptin was also the compound of choice to investigate further effects on uremic cardiomyopathy. This is of potential clinical impact, since patients with advanced stages of renal impairment are characterized by a high overall cardiac morbidity and mortality.
To analyze the temporal profile of TIMP-3 serum levels in SAH patients and their association with cerebral vasospasm
The main findings of this study are that: 1) MMP-9 and TIMP1 serum concentrations are significantly higher in SAH patients compared to healthy controls, 2) serum levels of MMP-9 and MMP-3 are significantly elevated in patients with dCVS compared to patients without dCVS, 3) this divergence starts in the very early phase of disease showing strongly differing values already on the second  day after bleeding, and 4) both, MMP-3 and TIMP-3 are significantly decreased during the first days after spontaneous SAH. Numerous studies suggest a crucial role of MMP-9 in the pathophysiology of aneurysmal SAH. Downregulation of proinflammatory mediators – including MMP-9 – was found to AZD2281 reduce the cerebrovascular inflammatory response and late cerebral ischemia after experimental SAH. MMP-9 is responsible for inactivation of plasma-type gelsolin, an antiinflammatory mediator. Decreased levels of plasma-type gelsolin have been found in SAH patients in combination with elevated cerebrospinal fluid levels of MMP-9. These findings suggest that one way of MMP-9 action in SAH is the inactivation of a sufficient anti-inflammatory response. Treatments aiming at the inhibition of neutrophil activity, including MMP-9 release, during the early phase after SAH have reduced microvascular injury and contributed to improved outcome after experimental SAH. The pivotal role of MMP-9 during the acute phase after SAH is underlined by animal studies using the MMP-9 antagonist minocycline, which has been shown to improve outcome after SAH in rats. Changes of MMPs and TIMPs in our patients might be attributable to an increased pro-inflammatory state after acute SAH. Inflammation cascades consist of a variety of factors, MMPs and TIMPs mirroring only a minor aspect of these complex pathways. However, major parameters associated with inflammation including WBCs, CRP and body temperature, have been controlled for indicating a predominant role of MMP-9, -3, TIMP-1 and -3 in the pathophysiology after aneurysmal SAH. Mean MMP-9 as wells as the MMP-9/TIMP-1 ratio were elevated in patients with dCVS in our study population. Data regarding the association of MMP-9 with the development of cerebral vasospasm are contradictory. Chou and colleagues did not find any association between MMP-9 levels and the occurrence of cerebral vasospasm. They report an elevation of MMP-9 during the first days after SAH. This is in contrast to our findings showing an increase of MMP-9 not only during the early phase after SAH, but also during later stages, when cerebral vasospasm has been found to be present. Interestingly, elevated levels of MMP-9 were not only associated with cerebral vasospasm in our study population but also with the presence of cerebral ischemia attributable to cerebral vasospasm. Yet, this association was not transferable to 6 month outcome. This might be a consequence of the limited number of patients with cerebral ischemia since an increase of MMP-9 has been described in numerous animal and clinical stroke studies underlining the importance of MMP-9 in cerebral ischemia. MMP-9 has a pivotal function as a cleavage molecule for a variety of proteins including the activation of Endothelin-1, which has been considered an important factor in the pathophysiology of cerebral vasospasm. Interestingly, LY2157299 Endothelin-1 leads to increased production of MMP-3 in astrocytes. In the present study patients with dCVS revealed significantly.
day after bleeding, and 4) both, MMP-3 and TIMP-3 are significantly decreased during the first days after spontaneous SAH. Numerous studies suggest a crucial role of MMP-9 in the pathophysiology of aneurysmal SAH. Downregulation of proinflammatory mediators – including MMP-9 – was found to AZD2281 reduce the cerebrovascular inflammatory response and late cerebral ischemia after experimental SAH. MMP-9 is responsible for inactivation of plasma-type gelsolin, an antiinflammatory mediator. Decreased levels of plasma-type gelsolin have been found in SAH patients in combination with elevated cerebrospinal fluid levels of MMP-9. These findings suggest that one way of MMP-9 action in SAH is the inactivation of a sufficient anti-inflammatory response. Treatments aiming at the inhibition of neutrophil activity, including MMP-9 release, during the early phase after SAH have reduced microvascular injury and contributed to improved outcome after experimental SAH. The pivotal role of MMP-9 during the acute phase after SAH is underlined by animal studies using the MMP-9 antagonist minocycline, which has been shown to improve outcome after SAH in rats. Changes of MMPs and TIMPs in our patients might be attributable to an increased pro-inflammatory state after acute SAH. Inflammation cascades consist of a variety of factors, MMPs and TIMPs mirroring only a minor aspect of these complex pathways. However, major parameters associated with inflammation including WBCs, CRP and body temperature, have been controlled for indicating a predominant role of MMP-9, -3, TIMP-1 and -3 in the pathophysiology after aneurysmal SAH. Mean MMP-9 as wells as the MMP-9/TIMP-1 ratio were elevated in patients with dCVS in our study population. Data regarding the association of MMP-9 with the development of cerebral vasospasm are contradictory. Chou and colleagues did not find any association between MMP-9 levels and the occurrence of cerebral vasospasm. They report an elevation of MMP-9 during the first days after SAH. This is in contrast to our findings showing an increase of MMP-9 not only during the early phase after SAH, but also during later stages, when cerebral vasospasm has been found to be present. Interestingly, elevated levels of MMP-9 were not only associated with cerebral vasospasm in our study population but also with the presence of cerebral ischemia attributable to cerebral vasospasm. Yet, this association was not transferable to 6 month outcome. This might be a consequence of the limited number of patients with cerebral ischemia since an increase of MMP-9 has been described in numerous animal and clinical stroke studies underlining the importance of MMP-9 in cerebral ischemia. MMP-9 has a pivotal function as a cleavage molecule for a variety of proteins including the activation of Endothelin-1, which has been considered an important factor in the pathophysiology of cerebral vasospasm. Interestingly, LY2157299 Endothelin-1 leads to increased production of MMP-3 in astrocytes. In the present study patients with dCVS revealed significantly.